In most solid tumors, large numbers of regulatory T (Treg) cells are linked to worse outcomes. These immune cells normally act as brakes on the immune system, which means they can weaken the body’s ability to attack cancer.
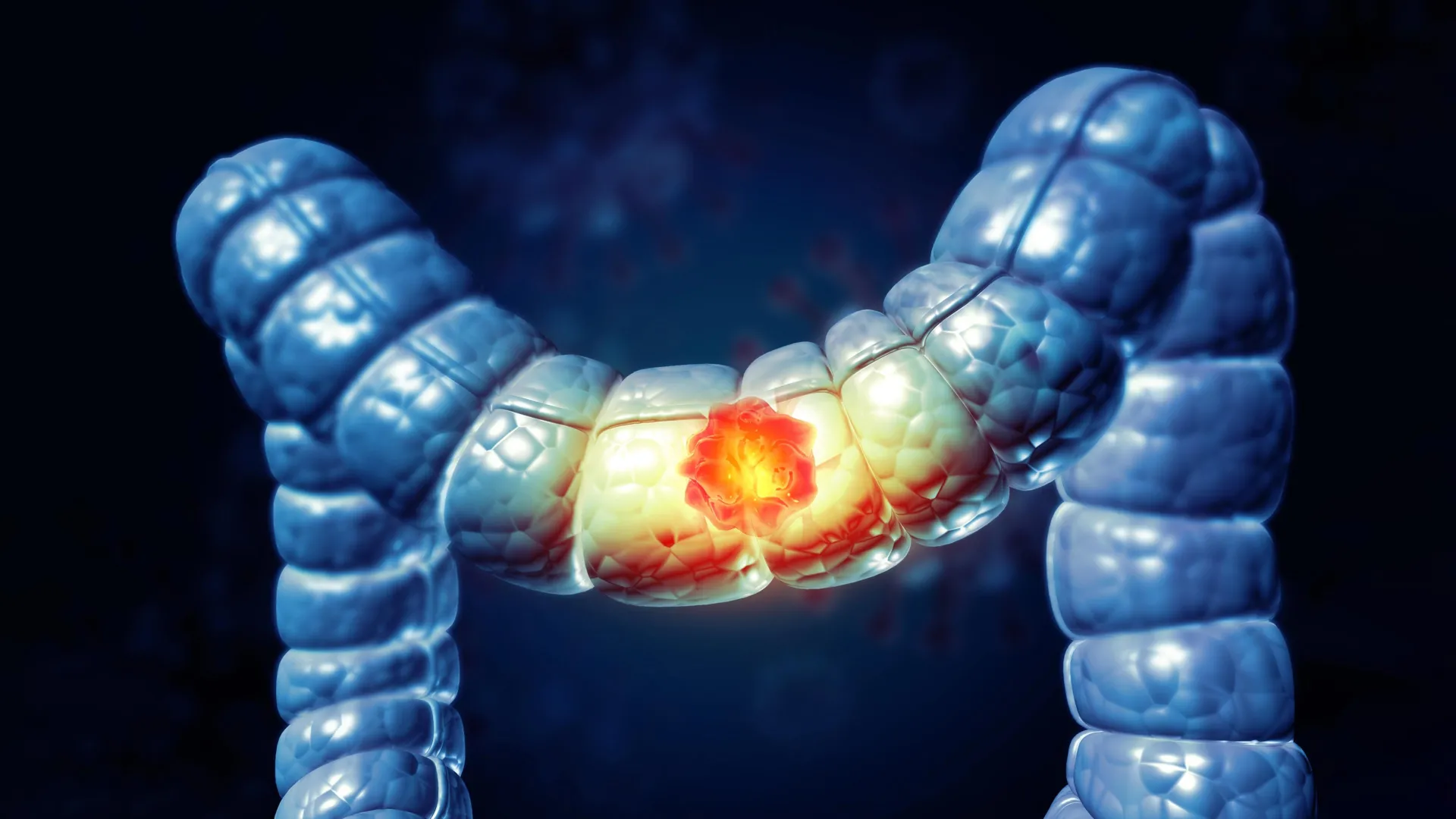
Colorectal cancer stands out as a rare and confusing exception. In this disease, tumors with more Treg cells are often associated with longer survival. For years, researchers have not understood why this pattern is so different from what is seen in other cancers.
A new study from researchers at the Sloan Kettering Institute at Memorial Sloan Kettering Cancer Center (MSK) now offers a clear explanation. The findings could help improve immunotherapy for most people with colorectal cancer and may also apply to cancers that develop in tissues like the skin and the lining of the stomach, mouth, and throat.
The key discovery is that Treg cells are not all the same. According to results published in the scientific journal Immunity, what matters most is not just how many Treg cells are present, but which kind they are.
“Instead of the regulatory T cells promoting tumor growth, as they do in most cancers, in colorectal cancer we discovered there are actually two distinct subtypes of Treg cells that play opposing roles — one restrains tumor growth, while the other fuels it,” says Alexander Rudensky, PhD, co-senior author of the study and chair of the Immunology Program at MSK. “It’s these beneficial Treg cells that make the difference, and this underscores the need for selective approaches.”
Decades of Research Lead to a Breakthrough
The study was led by first authors Xiao Huang, PhD, a postdoctoral researcher in the Rudensky Lab; Dan Feng, MD, PhD, a former MSK Medical Oncology fellow now at the Icahn School of Medicine at Mount Sinai; and Sneha Mitra, PhD, a postdoctoral researcher in the lab of computational biologist Christina Leslie, PhD, the study’s other senior author.
This work builds on more than 20 years of research by Dr. Rudensky, one of the world’s leading experts on regulatory T cells. His research helped establish that Treg cells maintain “immune tolerance.” This means they help the immune system distinguish between harmful threats and harmless targets, preventing unnecessary attacks on the body’s own cells, helpful microbes, and everyday foods.
Over time, his lab has also uncovered how Treg cells are created, how they function, and how they influence cancer development.
Focusing on the Most Common Form of Colorectal Cancer
Colorectal cancer is the second leading cause of cancer-related death when men and women are counted together, according to the American Cancer Society.
In this study, the researchers focused on the most common form of the disease, which accounts for about 80% to 85% of all colorectal cancers. These tumors are microsatellite stable (MSS) with proficient mismatch repair (MMRp), meaning their DNA remains relatively stable. Unfortunately, this group of cancers typically does not respond well to checkpoint inhibitor immunotherapies.
Earlier research at MSK showed that checkpoint inhibitors can be highly effective against the opposite tumor type. Cancers with high microsatellite instability (MSI-H) and mismatch repair deficiency (MMRd) can often be treated with immunotherapy alone, allowing many patients to avoid surgery, chemotherapy, and radiation.
Two Types of Treg Cells With Opposite Effects
To explore what makes common colorectal cancers different, the team used a mouse model developed at MSK that closely mirrors the genetic changes, behavior, and immune environment of human colorectal tumors.
They discovered that tumor-associated Treg cells fall into two main groups. One group produces a signaling molecule, or cytokine, called interleukin-10 (IL-10). The other does not.
By selectively removing each group in a series of detailed experiments, the researchers uncovered clear differences in how these cells affect tumor growth.
IL-10-positive Treg cells help slow tumor growth. They do this by reducing the activity of Th17 cells, another type of immune cell that produces interleukin 17 (IL-17). IL-17 acts as a growth signal for tumors. These protective Treg cells are more commonly found in healthy tissue near the tumor.
When IL-10-positive Treg cells were removed, tumors grew more quickly.
IL-10-negative Treg cells had the opposite effect. These cells suppress powerful immune defenders, especially CD8+ T cells that are known for their cancer-fighting abilities. This harmful subtype is mainly found inside the tumor itself.
When IL-10-negative Treg cells were eliminated, tumors became smaller.
Patient Data Confirms the Findings
The team confirmed these results using tumor samples from people with colorectal cancer. In these samples, they again identified two distinct populations of IL-10-positive and IL-10-negative Treg cells.
They also analyzed outcomes for more than 100 colorectal cancer patients. Those with higher levels of the beneficial IL-10-positive Treg cells lived longer. Patients whose tumors contained more IL-10-negative Treg cells had poorer outcomes.
“This research shows how important these positive cells are,” Dr. Huang says. “And it highlights the need to develop therapies that can selectively eliminate the harmful Tregs while preserving the helpful ones.”
Targeting CCR8 as a New Treatment Strategy
The findings suggest a promising path forward for improving treatment for most colorectal cancer patients, according to Dr. Rudensky, who is also a Howard Hughes Medical Institute Investigator.
The researchers found that IL-10-negative Treg cells express high levels of a protein called CCR8. These cells are the ones that suppress the immune response and are primarily located within tumors.
Earlier work from Dr. Rudensky’s lab, led by breast cancer surgeon George Plitas, MD, showed that CCR8 is also highly expressed on tumor Treg cells in breast cancer and many other human cancers. That research suggested that antibodies could be used to selectively remove harmful Treg cells. Doing so could allow the immune system to attack tumors more effectively while leaving beneficial Treg cells intact.
“This idea of using CCR8-depleting antibodies, which was pioneered at MSK, is the main target of global efforts to bring regulatory T cell-based immunotherapy to the clinic,” Dr. Rudensky says.
Multiple clinical trials are now testing this approach at MSK and other institutions, both on its own and in combination with existing immunotherapies. The new study strengthens the case for using this strategy in colorectal cancer and possibly beyond.
Similar Immune Patterns in Other Cancers
The researchers also examined a large dataset of T cells from 16 different cancer types to see whether the same immune patterns appeared elsewhere. They found similar divisions between IL-10-positive and IL-10-negative Treg cells in several cancers affecting the skin and the lining of the mouth, throat, and stomach.
“What these tissues have in common is that immune cells play a critical role in constantly defending and repairing them as they’re exposed to microbes and environmental stresses,” says Dr. Mitra, who led the data analysis and is co-mentored by Dr. Leslie and Dr. Rudensky.
The team suggests that therapies designed to remove IL-10-negative Treg cells in colorectal cancer might also work against these other cancers that arise in barrier tissues.
A Different Immune Balance in Metastatic Disease
When the researchers studied colorectal cancer that had spread to the liver, they observed a different immune pattern.
In these metastatic tumors, IL-10-negative Treg cells greatly outnumbered the helpful IL-10-positive cells. Unlike primary tumors, removing all Treg cells in this context caused metastatic tumors to shrink.
This result highlights the need for treatment strategies that account for both the tissue involved and the stage of disease, the researchers say.
Authors, Funding, and Disclosures
Additional authors include Emma Andretta, Nima Hooshdaran, Aazam Ghelani, Eric Wang, Joe Frost, Victoria Lawless, Aparna Vancheswaran, Qingwen Jiang, Cheryl Mai, and Karuna Ganesh.
The Integrated Genomics Operation and the Single Cell Research Initiative at MSK played key roles in the research.
Funding was provided by the National Cancer Institute (P30 CA008748, U54 CA274492, T32 CA009512), the National Institute of Allergy and Infectious Diseases (AI034206), the Ludwig Center for Cancer Immunotherapy at MSK, the Howard Hughes Medical Institute, the Cancer Research Institute, and a Marie-Joseé Kravis Fellowship in Quantitative Biology.
Dr. Rudensky serves on scientific advisory boards and holds equity in Sonoma Biotherapeutics, RAPT Therapeutics, Coherus Oncology, Santa Ana Bio, Odyssey Therapeutics, and Nilo Therapeutics. He is also a scientific advisory board member of Amgen, BioInvent, and Vedanta Biosciences, has consulted for AbbVie, and serves as an editor of the Journal of Experimental Medicine and an editorial advisor to Immunity.
Dr. Rudensky and Dr. Plitas are inventors on patents and patent applications held by MSK related to CCR8-based therapeutic depletion of tumoral Treg cells and novel antibodies against CCR8.