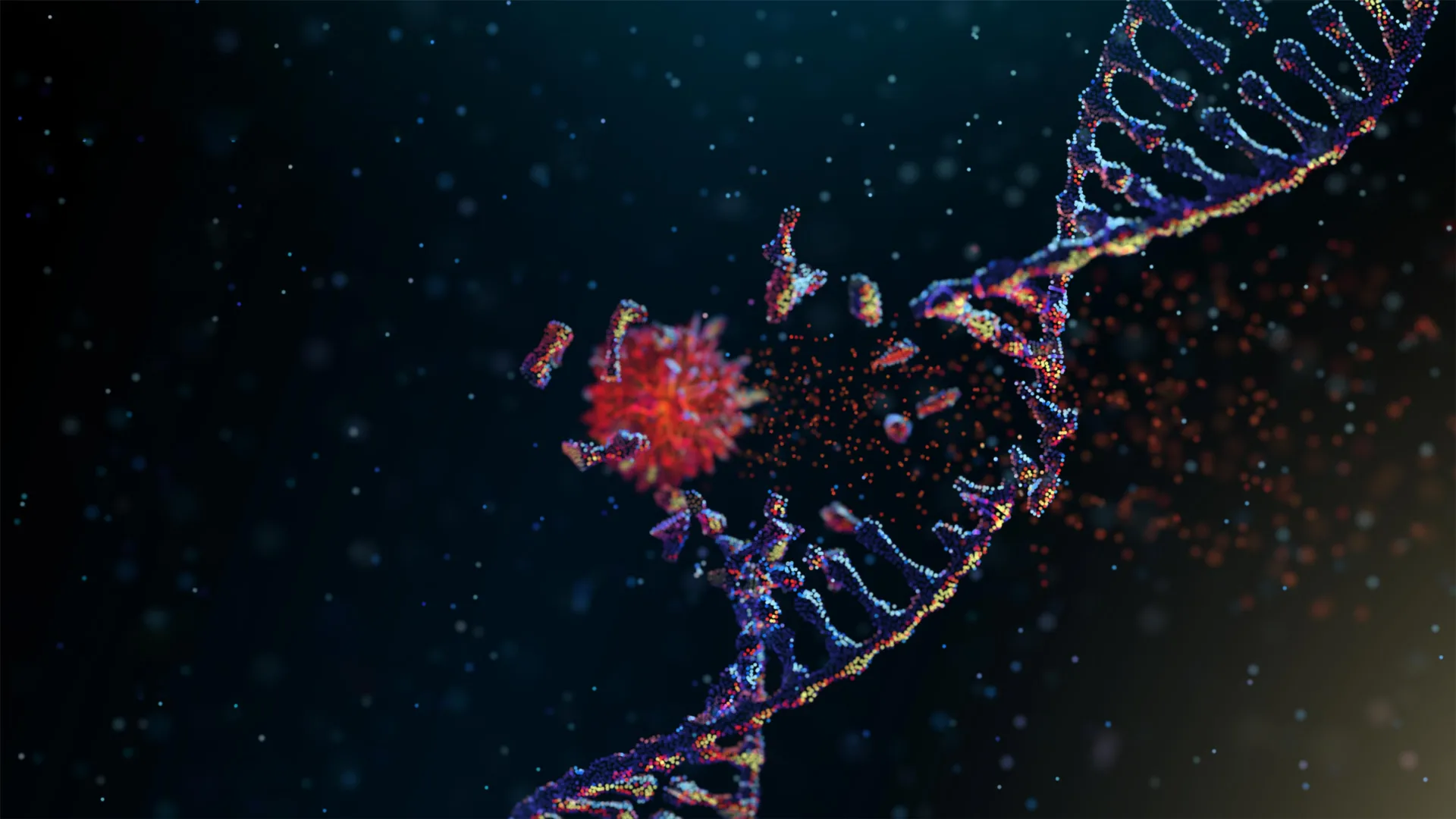
Scientists at the University of California San Diego have identified the enzyme responsible for chromothripsis, a dramatic genetic event in which a chromosome breaks into many fragments and is stitched back together in the wrong order. This chaotic reshuffling allows cancer cells to evolve quickly and develop resistance to treatment. Although chromothripsis was first recognized more than ten years ago as a major force in cancer progression, researchers had not known what actually set it in motion. The new findings, published in Science, uncover the cause and point to potential new strategies for treating some of the most aggressive cancers.
Cancer cells use several tactics to survive therapy, but chromothripsis stands out because of its sheer scale. Rather than building up mutations gradually over time, this process can create dozens or even hundreds of genetic alterations in a single catastrophic episode. The result is a rapid burst of evolution that can make tumors harder to control.
Chromothripsis is also surprisingly common. Studies suggest that about one in four cancers shows signs of this type of chromosome damage, and in some cancers the rate is even higher. Nearly all osteosarcomas, an aggressive bone cancer, display evidence of chromothripsis, and many brain cancers show especially elevated levels.
“This discovery finally reveals the molecular ‘spark’ that ignites one of the most aggressive forms of genome rearrangement in cancer,” said senior author Don Cleveland, Ph.D., professor of cellular and molecular medicine at UC San Diego School of Medicine and member of UC San Diego Moores Cancer Center. “By finding what breaks the chromosome in the first place, we now have a new and actionable point of intervention for slowing cancer evolution.”
How N4BP2 Breaks DNA Inside Micronuclei
Chromothripsis begins when errors during cell division trap individual chromosomes inside small, fragile compartments known as micronuclei. When a micronucleus ruptures, the chromosome inside is left exposed. At that point, it becomes vulnerable to nucleases, enzymes that can cut DNA strands.
Until now, researchers did not know which nuclease was responsible for triggering this destructive chain reaction, making it impossible to design therapies aimed at stopping it.
To pinpoint the culprit, the team used an imaging based screening approach to systematically examine all known and predicted human nucleases. They monitored how each enzyme behaved in living cancer cells. One enzyme, N4BP2, stood out. It was uniquely able to enter micronuclei and fragment the DNA inside.
The researchers then tested whether N4BP2 directly causes chromothripsis. When they removed the enzyme from brain cancer cells, chromosome shattering dropped dramatically. In contrast, when they forced N4BP2 into the cell nucleus, intact chromosomes broke apart, even in otherwise healthy cells.
“These experiments showed us that N4BP2 isn’t just correlated with chromothripsis. It is sufficient to cause it,” said first author Ksenia Krupina, Ph.D., a postdoctoral fellow at UC San Diego. “This is the first direct molecular explanation for how catastrophic chromosome fragmentation begins.”
Link to Aggressive Tumors and Extrachromosomal DNA
The team also examined more than 10,000 cancer genomes spanning multiple tumor types. Cancers with higher levels of N4BP2 activity showed significantly more chromothripsis and large scale structural rearrangements. These tumors also had increased amounts of extrachromosomal DNA (ecDNA), circular DNA fragments that often carry cancer promoting genes and are closely associated with aggressive growth and resistance to therapy.
Tumors rich in ecDNA are among the most difficult to treat. As a result, ecDNA has drawn major scientific interest and has been named one of the Cancer Grand Challenges by the National Cancer Institute and Cancer Research UK. The new findings suggest that ecDNA is not a separate phenomenon but rather a downstream consequence of chromothripsis. By placing N4BP2 at the very start of this process, the study highlights a key entry point for understanding and potentially controlling some of the most unstable and dangerous forms of cancer genome instability.
“Understanding what triggers chromothripsis gives us a new way to think about stopping it,” said Cleveland. “By targeting N4BP2 or the pathways it activates, we may be able to limit the genomic chaos that allows tumors to adapt, recur and become drug-resistant.”
Additional coauthors of the study include Alexander Goginashvili, Michael W. Baughn, Stephen Moore, Christopher D. Steele, Amy T. Nguyen, Daniel L. Zhang, Prasad Trivedi, Aarti Malhotra, David Jenkins, Andrew K. Shiau, Yohei Miyake, Tomoyuki Koga, Shunichiro Miki, Frank B. Furnari and Ludmil B. Alexandrov, all at UC San Diego and Jonas Koeppel and Peter J. Campbell of the University of Cambridge and the Wellcome Trust Sanger Institute.
The study was funded, in part, by the National Institutes of Health (grants R35GM122476, R01 ES030993-01A1, R01ES032547-01, U01CA290479-01, R01CA269919-01, R56 NS080939 and R01 CA258248).